PPP-58: Adapting a Prescription
| Policy |
|---|
The College of Pharmacists of BC’s Professional Practice Policy 58 Adapting a Prescription (PPP-58) provides the framework to guide pharmacists in safely and effectively adapting existing prescriptions, enabling them to use their professional judgement to change the dose, formulation, or regimen of a prescription; renew a prescription for continuity of care; and make therapeutic drug substitutions. PPP-58 is applicable to pharmacists in all practice settings including community, long-term care, hospital, and other institutional pharmacy settings.
Adaptation activities in PPP-58 are enabled under the Health Professions Act.
It is not mandatory that a pharmacist adapt a prescription and the decision to adapt a prescription is at the discretion of the individual pharmacist. Should a pharmacist choose to adapt a prescription however, the intent must be to optimize therapeutic outcome of treatment and the adaptation must be done in accordance with PPP-58 and within the limits of the pharmacist’s own competencies.
This authority allows pharmacists to demonstrate their value, as medication experts, in an evolving client-centered, clinical care environment.
FAQs
- What constitutes 'appropriate knowledge and understanding of the condition and the drug being dispensed' for pharmacists adapting prescriptions?
A pharmacist must use their professional judgement to determine if they have the ‘appropriate knowledge and understanding of the condition and the drug being dispensed’ each time they consider adapting a prescription, as each situation can be unique.
- What constitutes 'sufficient information about health status' for a pharmacist to adapt a prescription safely?
A pharmacist must use their professional judgement to determine if they have ‘sufficient information’ specific to the client each time they consider adapting a prescription.
In doing this, a pharmacist must ensure they review all relevant information that is available to them. This would include, but is not limited to, a review of the client’s local and PharmaNet record, any client specific information conveyed by the prescriber and any information obtained directly from the client or their representative.
- What does it mean that a pharmacist must not adapt an expired prescription or extend a prescription beyond its original expiry date?
All prescriptions (new and existing) are valid for up to TWO years from the prescribing date, with exception of prescriptions for benzodiazepines and other targeted substances, which are valid for a period of up to ONE year from the prescribing date (unless validity up to two years is permitted by a section 56 exemption to the Controlled Drugs and Substances Act).
For example, a prescription issued on January 5, 2022 that is valid for two years would expire on January 4, 2024. After January 4, 2024, this prescription would no longer be valid, regardless of how many refills were initially authorized by the prescriber, and would not be eligible for adaptation.
A pharmacist must ensure that the duration of the adaptation does not exceed the expiry date of the prescription. In this example, the pharmacist would only be able to authorize a quantity that would supply the client up to, and not beyond, January 4, 2024.
- Do I have to use the adaptation documentation and notification template form on the College website, or can I use my own template?
Documentation and notification of adaptations must meet the requirements listed in part 3(f) and (g) of PPP-58. A pharmacist can choose to use their own templates but must ensure that all the required information is documented and retained as part of the client’s record.
- Why is it important to document an adaptation?
Documentation establishes accountability and responsibility for performing prescription adaptations. It is an important component in demonstrating how the pharmacist exercised their professional judgement through documentation of their rationale and case-specific details that support the pharmacist’s decision to adapt.
Some tips for documentation include:
- Complete your documentation as soon as possible (preferably immediately) after the activity
- Ensure all required information is documented as per part 3(f) of PPP-58
- Include all relevant information deemed necessary to support the decision to perform an adaptation
- Ensure all documentation is legible and non-erasable
- Do not delete, remove or rewrite any part of the adaptation record. If you make an error, cross out the error with a single line and initial it
- How is providing an emergency supply for continuity of care under PPP-31 different than providing a renewal under PPP-58?
Under PPP-58, pharmacists can utilize their professional judgement to adapt (renew) a prescription, for whatever period of time they feel is appropriate for non controlled substances, as long as the duration does not exceed the expiry of the prescription. When adapting, the pharmacist must ensure they have sufficient knowledge, understanding and client-specific information to determine if the adaptation and subsequent continuation of therapy is in the best interest of the client. Adapted renewals are generally performed when a pharmacist decides that they have enough information to determine a longer-term supply may be in the best interest of the client.
PPP-31 allows pharmacists to provide clients with an emergency supply of prescription drugs for continuity of care in exceptional circumstances. Although this policy gives broad latitude for pharmacists to exercise their professional judgement, generally, emergency supplies are utilized to provide short term supplies when a renewal does not meet the criteria in PPP-58.
A pharmacist may opt for providing an emergency supply rather than an adapted renewal for several reasons, including:
- The pharmacist is not comfortable providing a longer-term supply based on the client’s health status.
- The prescription does not qualify for adaptation under PPP-58.
- The client has an upcoming appointment with their prescriber to obtain a new prescription.
- It is not in the patient's best interest to provide an adapted renewal.
- What is NOT considered a prescription adaptation?
- Contacting the Original Prescriber for Changes:
If a pharmacist identifies a drug-therapy problem and contacts the original prescriber to discuss changes, any adjustments authorized by the prescriber are not considered adaptations. This is because the pharmacist is seeking prescriber authorization prior to dispensing rather than making an independent adaptation decision.
- Following Hospital-Approved Protocols:
In environments where a hospital governing body has approved a therapeutic interchange program or a protocol intended to optimize therapeutic outcomes, any prescription changes made in accordance with this program or protocol do not count as adapting.
- Providing Emergency Supplies:
If the situation/issue presented does not meet the requirements for an adaptation under PPP-58, the pharmacist may consider providing emergency supplies to the client to ensure continuity of care under PPP-31.
- Dispensing Interchangeable Drugs:
Dispensing an “interchangeable drug” as defined in the Health Professions Act is not adaptation. Any changing of formulation in the dispensing of interchangeable drugs (i.e., generic products) is being done for a different purpose than formulation changes permitted in adapting.
- Contacting the Original Prescriber for Changes:
- Do I always need to obtain consent to adapt a prescription? Do I need to document consent?
In BC, the obligation to obtain informed consent to healthcare from an adult client, the criteria for consent, and how to obtain consent, is set out in the Health Care (Consent) and Care Facility (Admission) Act.
That Act states that every adult client has the right to give, refuse or withdraw consent to treatment. Providing treatment by adapting a prescription in accordance with PPP-58 requires the pharmacist to obtain consent from the particular client.
In BC, the age of majority is 19 years. A person who has not reached the age of majority may be described as a “minor” or an “infant”. Usually, a parent or guardian provides consent to healthcare on behalf of the minor. However, this is not always the case. In BC there is no set age when a minor is considered capable to give consent independent of their parents’ or guardians’ wishes. Section 17 of the Infants Act provides that a minor may consent to treatment if the pharmacist has explained the nature, consequences, and reasonably foreseeable risks and benefits of the treatment to the minor and is satisfied that the minor understands them. The pharmacist must also determine that the treatment is in the minor's best interest. This is often referred to as “mature minor consent”. A parent or guardian cannot overrule the mature minor’s decision and, under the Personal Information Protection Act, a parent or guardian is not entitled to disclosure of information about the treatment without the mature minor’s consent.
Consent may be expressed verbally, in writing, or may be inferred from the client’s conduct. PPP-58 requires the pharmacist to document the acknowledgement of informed consent for all clients regardless of client age.
- Can I provide a renewal for narcotic, controlled drug or targeted substance under PPP-58?
Yes, but only if permitted under a section 56 exemption to the Controlled Drugs and Substances Act. The pharmacist may use their professional judgement to determine if they have the appropriate knowledge and if it is in the client’s best interest to provide an adapted renewal of a narcotic, controlled drug or targeted substance.
Renewals for narcotics, controlled drugs, or targeted substances must not exceed the prescription's expiry date and must not be for a duration longer than either the originally prescribed period or 30 days, whichever is greater.
- Can a pharmacist adapt a prescription that has been previously adapted?
Yes. There is no limit on the number of times a prescription may be adapted in accordance with PPP-58, as long as the prescription, at the time of each adaptation, is current, authentic, and valid.
Every adaptation is a new adaptation of the prescription. This means that when adapting a previously adapted prescription, the pharmacist must locate and refer to the prescription issued by the practitioner within their pharmacy management software system.
- Can I transfer an adaptation from one pharmacy to another?
A prescription that has been adapted previously may be transferred to a different pharmacy in accordance with the Health Professions Act Bylaws Schedule F, Part 1. An adaptation does not create a new prescription, as such, the adaptation alone cannot be transferred—it must be attached to a prescription.
It is important to note that adapted prescriptions for narcotics, controlled drugs, or targeted substances can only be transferred if allowed under:
a) The Controlled Prescription Program, if applicable to the specific narcotic, controlled drug, or targeted substance.
b) A section 56 exemption to the Controlled Drugs and Substances Act.
Under the HPA Bylaws Community Pharmacy Standards of Practice, if a prescription has no refills remaining then it cannot be transferred to another pharmacy, and no further adaptations (including renewal for continuity of care) of that prescription can be made at the receiving pharmacy.
- Can I adapt (renew) a prescription with no refills at a different pharmacy?
No. A prescription with no refills remaining, cannot be transferred to another pharmacy. See Health Professions Act Bylaws Community Pharmacy Standards of Practice.
- Can I adapt a prescription from a prescriber who is no longer practicing (e.g., retired, suspended)?
Yes. A pharmacist may adapt a prescription from a prescriber who is no longer practicing, whether due to retirement, suspension, or other limits and conditions on their prescribing authority. See Policy Statement 6 in PPP-58.
- Can the pharmacist make more than one modification to a prescription when adapting (e.g., changing the dose and dosage form at the same time)?
Yes. A pharmacist can make more than one modification in a single adaptation, if based on their judgement, it is deemed clinically appropriate to do so.
- How do I determine whether renewing a client’s prescription is appropriate?
A pharmacist must use their professional judgement to guide their client-specific decisions when renewing a prescription. Generally, this requires that the pharmacist be reasonably satisfied that there has been no clinically significant change to the prescription for at least 3 to 6 months, and the condition being treated is stable.
- A client was prescribed M-Eslon 10 mg once daily at bedtime (quantity authorized in prescription: 30 capsules), but requested to change it to M-Eslon 5 mg twice daily. Can I adapt the prescription to make the change?
Yes. As long as the quantity dispensed does not exceed the stated amount authorized in the prescription, the pharmacist may utilize PPP-58 if the adaptation benefits the client (Policy Statement 13.b.ii). When the pharmacist adapts to 5mg twice daily, the pharmacist may dispense up to 60 capsules of the 5mg dose.
Practical Examples
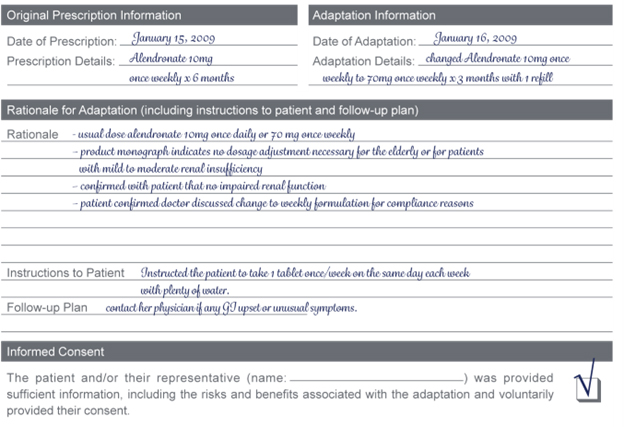
- Changing the Dose
You receive a new prescription for alendronate 10mg once weekly for an elderly female patient. The PharmaNet record indicates the patient was previously taking alendronate 10mg once daily for the past year. You have a discussion with the patient and determine the following:
- The patient has been having difficulty with compliance of the once daily regimen.
- The physician discussed with her that she was changing the prescription to the once weekly formulation to make it easier for her to remember her dose.
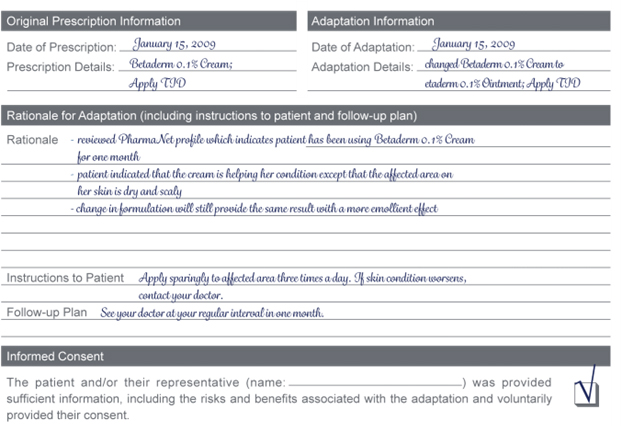
- Changing Formulation
You receive a new prescription for an adult female patient for Betaderm 0.1% Cream; Apply TID. The patient indicated that her skin is really dry and scaly and that she would prefer a product with more of a moisturizing effect.
You have a discussion with the patient and determine the following:
- She had used Betaderm 0.1% Cream for one month and was getting results with the cream.
- You visually confirm that her skin is dry and scaly.
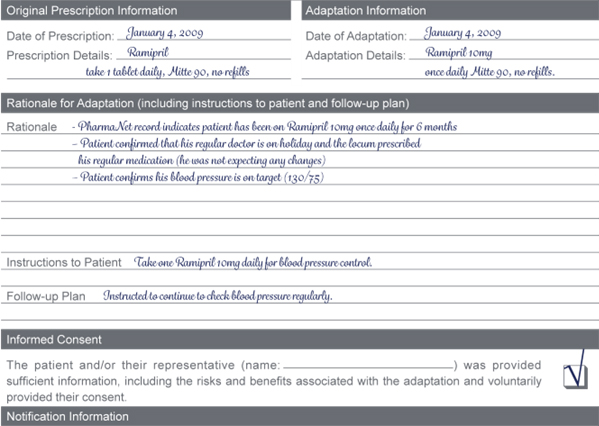
- Incomplete Information
You receive a new prescription for Ramipril – take one tablet daily. No strength is indicated on the prescription. The PharmaNet record indicates the patient has been getting the 10mg strength for the past 6 months.
You have a discussion with the patient and determine the following:
- The patient confirms that the prescription was intended for the same dose (10mg) as before and that the medication is being used for blood pressure control.
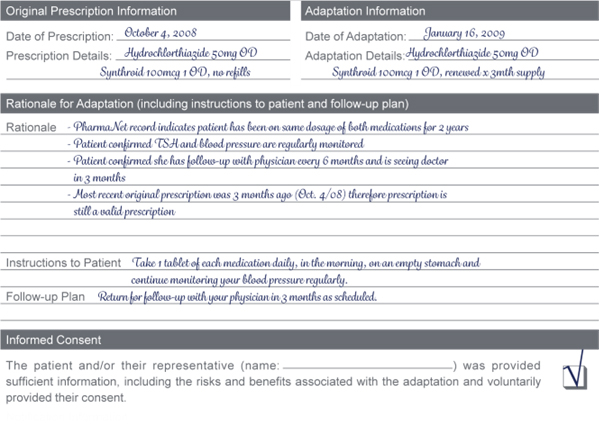
- Renew a Prescription
A long standing patient of your pharmacy takes a thyroid supplement and diuretic every day. She comes to the pharmacy and requests a renewal of her prescriptions. You notice in your records that 3 months ago she received the same prescriptions but no refills were authorized. You review the PharmaNet record and determine she has been on the same dose of the same medications for 2 years.
You have a discussion with the patient and determine the following:
- She confirms that her TSH levels are being regularly monitored as well as her blood pressure.
- She confirms that she sees her physician every 6 months and that she is due for her follow-up in 3 months.
- Therapeutic Substitution
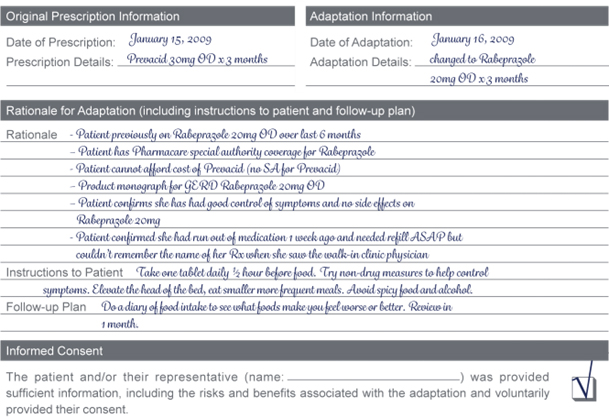
Patient arrives at your pharmacy with a prescription for Prevacid 30mg once daily x 3 months for GERD. You notice the prescription is from the local walk-in clinic physician. You check the PharmaNet profile and determine that the patient has previously been on Rabeprazole 20mg once daily x 6 months and has had Pharmacare coverage through special authorization for the Rabeprazole. You process the prescription for Prevacid 30mg once daily and notice that the patient does not have special authorization for the Prevacid.
You have a discussion with the patient and determine the following:
- The patient receives social assistance and cannot afford the prescription cost for the Prevacid.
- The patient had run out of the Rabeprazole prescription last week and couldn’t get to her regular doctor, so went to the walk-in clinic.
- The patient wanted a renewal of the prescription she was previously on for her heartburn, but she couldn’t remember the name of it when she went to the clinic and she didn’t have her empty vial with her.
- Her previous prescription had been controlling her symptoms very well and she had not had any side effects.
- Patient is anxious to get her Rabeprazole medication as her symptoms have increased over the past week since she has been out of her medication.
Note: In the ‘Notification’ section of the form you would indicate that both physicians were notified of this adaptation.
 Share
Share